(BlackDoctor.org) — A new study hints at one reason that black Americans are at a higher risk of death from heart disease than whites: Blacks appear to have higher levels of a certain type of plaque that builds up in arteries and is not detected in standard screening.
(BlackDoctor.org) — A new study hints at one reason that black Americans are at a higher risk of death from heart disease than whites: Blacks appear to have higher levels of a certain type of plaque that builds up in arteries and is not detected in standard screening.
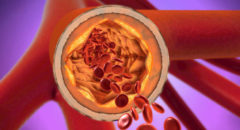
This so-called “non-calcified plaque” — which consists of soft deposits that accumulate deep in the walls of arteries — can rupture and send out blood clots that can lead to heart attacks.
The new study looks specifically at non-calcified plaque, not calcified plaque, which is commonly monitored in coronary screening tests. The study authors said ordinary calcium screening tests such as CT scans may not be as valid for blacks since they miss the non-calcified plaque.
“For a long time, physicians have searched for explanations as to why African Americans have higher rates of heart disease and higher cardiac death rates, but less coronary artery calcium than Caucasians,” said study co-author Dr. U. Joseph Schoepf, professor of radiology and medicine and director of cardiovascular imaging at the Medical University of South Carolina in Charleston, in a news release. “We show that one possible explanation for the discrepancy may be found in the higher rate of less stable, non-calcified plaque in the heart vessels of African Americans.”
Federal statistics show that blacks are more likely than whites to be diagnosed with heart disease and die of it.
In the study, researchers screened 301 patients for both kinds of plaque using two kinds of technology: CT and contrast-enhanced coronary CT angiography technology. (The latter allows monitoring of different kinds of plaques.) Half the patients were black and half were white, and a third were male. The average age was 55.
Researchers found that non-calcified plaque was much more common in black patients: 64 percent of them had it, compared to 41 percent of whites. Blacks also had more of the plaque in their arteries.
Whites, on the other hand, were more likely to have higher levels of calcified plaque than blacks (45 percent vs. 26 percent).
Dr. Keith Ferdinand, chief science officer of the Association of Black Cardiologists, said it’s important to remember that CT angiography is not a perfect test, especially in patients with diabetes and obesity, which are common among blacks.
Ferdinand added that it’s difficult to pinpoint the specific effect that race has upon health — as this study attempts to do — considering how many differences that may exist between different racial groups.
The study appears in the journal Radiology.