When it comes to heart disease, health statistics tend to focus a lot on men and their particular health risks. But looking at the statistics in another way, African-American women are 35 percent more likely to die of heart disease than Caucasian women, and surveys show they are far less aware of their risk factors.
When it comes to heart disease, health statistics tend to focus a lot on men and their particular health risks. But looking at the statistics in another way, African-American women are 35 percent more likely to die of heart disease than Caucasian women, and surveys show they are far less aware of their risk factors.
Heart disease is the leading cause of death for women of most racial/ethnic groups in the United States, including African Americans, American Indians or Alaska Natives, Hispanics, and whites. For Asian American women, heart disease is second only to cancer.
In 2006, about 6.9% of all white women, 8.8% of black women, and 6.6% of Mexican American women were living with coronary heart disease.
Black women develop hypertension earlier in life and have higher average blood pressure than white women, according to HHS. Nearly half of black women have a total cholesterol number that is way too high. Nearly 80 percent are overweight or obese.
About 450,000 women suffer heart attacks each year; in fact, cardiovascular disease is the No. 1 killer in the U.S. But the good news is that more women are surviving heart attacks. Read up on 5 heart health myths that put women at risk. Plus, test your heart health IQ with our quiz…
First, the good news: More women are survivng heart attacks. About 5% of women under age 55 died of a heart attack in 1994, but in 2006 that number went down to 2.4%. But the bad news? Younger women are still less likely to survive a heart attack than are men.
The Top Myths Putting Women’s Hearts At Risk
Myth 1. The pain is in my arm, not my chest, so I don’t have to worry.
Women die from heart attacks because they often don’t recognize the symptoms until it’s too late. Until recently, many healthcare providers also missed heart attacks in women (and still do occasionally) because women don’t always have the same symptoms as men do.
Men usually have heaviness in the left side of their chest, a feeling that’s often described as having an elephant sitting on top of them. It can be accompanied by pain down the left arm or up the neck, sweating and shortness of breath.
Some women do have the same symptoms as men. But many women having a heart attack don’t have chest pain at all. They may have jaw, arm, back or stomach pain or an overwhelming feeling of fatigue, along with shortness of breath. Or they may feel as if they have a bad flu and may experience nausea and vomiting.
Most women experience symptoms about a month before the heart attack, according to a study by the National Institutes of Health. The most common warning signs were unusual fatigue, sleep problems, shortness of breath, indigestion and anxiety.
Women have great instincts, particularly about their own bodies. If you know that you are more tired than usual or simply are not feeling like yourself, especially if you have one or more risk factors for heart disease, see your doctor as soon as possible.
If you think you’re having a heart attack, call 911 immediately. While waiting for the ambulance, chew an aspirin (an adult 325 mg dose or two baby aspirins). Don’t take aspirin if you are allergic to it.
Once the ambulance arrives, the paramedics will begin treatment immediately. Don’t go to the emergency room on your own; it will delay treatment. Time is crucial – the earlier you’re treated, the better your chances of maintaining healthy heart muscle and recovering quickly.
Myth 2. I have to stay away from all fats.
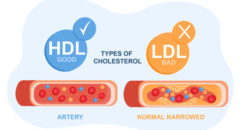
For years, the emphasis was on the importance of a low-fat diet, especially for heart health. It’s no wonder that when many people hear the word “fats,” they think “unhealthy.”
But some fats are actually good for us. New dietary recommendations from the American Heart Association consider “good” and “bad” fat which, thankfully, leads to a much tastier way of eating.
What exactly are “fats”? Unsaturated fats are “good” fats, coming mostly from plant or vegetable sources, and not from red meat. Examples are olive oil, flaxseed oil and fish oil (such as from salmon).
Saturated fats and trans fats are bad for our hearts. Saturated fats are mostly from animal sources, such as meat and full-fat dairy products. Trans fats are man-made; manufacturers add hydrogen to vegetable oil to increase the flavor and the shelf life. These are found in many snack foods (potato chips, cookies, cakes), margarine, vegetable shortenings and some fried foods.
“Good” fats should be incorporated into our daily diets. Cooking with olive oil, sprinkling ground flaxseed on yogurt or cereal, and eating wild salmon are easy ways to do this.
Avoid or limit your intake of saturated and trans fats. Use low-fat dairy products (or those labeled “no fat”), limit the amount of red meat you eat, and avoid margarine, fried foods and snack foods. You’ll help your heart, stay at a healthy weight and feel better!
Myth 3. My life is very busy and very stressful, so a heart attack is inevitable.
Although a lot of attention has been paid to the negative health effects of the hard-driving, high-stress lifestyle, many studies have shown having a Type A personality alone does not mean a higher incidence of heart disease. But some factors associated with a Type A personality – high blood pressure, smoking and lack of exercise – are risk factors.
Feelings associated with an increased risk are depression, a negative outlook, and anger and hostility.
So make mental and spiritual health a priority. Get help for depression and feelings of constant anger and hostility. Connect with others to improve your sense of well being.
Of course, eating a healthy diet and exercising regularly are extremely important for physical and mental health.
Myth 4. Only middle-aged people have heart attacks.
Actually, most women are only protected (relatively) from heart disease until menopause. But premenopausal women with diabetes, a genetic form of high cholesterol (known as familial hyperlipidemia), untreated high blood pressure, and those who smoke or are overweight, are especially at risk for heart disease, no matter their age.
Women in their 20s, 30s, 40s and 50s have heart attacks. And they’re often misdiagnosed because no one expects a young woman to have a heart attack, especially because she may not have the typical symptoms.
Myth 5. My weight and cholesterol are normal, so I’m not at risk for heart disease.
Maintaining a healthy weight and having normal total cholesterol levels are important for artery health, but these factors aren’t enough to guarantee heart health. Other risk factors increase your chances of developing coronary artery disease (CAD). Some can be changed; others can’t.
Risk factors that can’t be changed include: getting older, gender, heredity and having had a prior heart attack or stroke. Risk increases as you age. Men are more at risk than pre-menopausal women; after menopause, women are equally at risk. Having a family member with heart disease or who has had a heart attack at an early age is a major risk factor.
Risk factors that can be changed are high blood pressure, diabetes, cigarette smoking, a sedentary lifestyle, stress and depression, hormone replacement therapy in older women, high total cholesterol and being overweight.
Even if your weight and cholesterol are normal, if you have even one other risk factor, such as high blood pressure or a family history of coronary artery disease, then you’re still at risk. You need to take into account all these factors to get an accurate picture of your risk.
Easy Ways To Lower Heart Attack Risks
- Have your blood pressure checked regularly.
- Ask your doctor to test your blood glucose and total cholesterol levels.
- Stop smoking now!
- Start exercising regularly.
- Talk to your doctor about stress reduction and options to control depression.
Also, discuss hormone replacement therapy after menopause; it should be taken for a limited time, and some women should not take it at all. Find out if anyone in your family has had a heart attack, or CAD, and let your doctor know. If you know your risk factors for heart disease, then you have the power to keep yourself heart healthy.