Ischemic stroke patients who have recurrent asymptomatic brain lesions within
Ischemic stroke patients who have recurrent asymptomatic brain lesions within
three months of their initial stroke are at increased risk for subsequent
strokes, says a U.S. study in the December issue of the journal Archives of
Neurology.
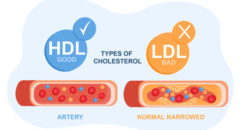
An ischemic stroke
occurs as a result of inadequate blood flow to the brain.
Previous research
found that asymptomatic (silent) brain lesions — changes in brain tissue that
occur in areas where blood flow is blocked or reduced — occur more frequently
than symptomatic lesions up to three months after a stroke, according to
background information in the article.
The authors of this
current study investigated whether silent brain lesions detected by MRI scans
could help predict stroke patients’ risk for subsequent
strokes.
Researchers at the
National Institute of Neurological Disorders and Stroke studied 120 ischemic
stroke patients. Each patient had an MRI brain scan within 24 hours of the
stroke and five days after the stroke. Of those patients, 68 had a follow-up MRI
after 30 days or up to 90 days after the stroke.
The study found that
patients who had silent ischemic lesions on the 30- or 90-day MRI were about 6.5
times more likely than other patients to suffer a subsequent ischemic stroke.
Patients with silent lesions on any of the MRI scans (24 hours, five days, 30
days, or 90 days) had an increased risk of death from vascular causes, recurrent
ischemic stroke or transient ischemic attack.
“It is a matter of circumstance, rather than tissue pathological
features, that determines whether cerebral ischemia is symptomatic or silent,”
the study authors wrote. “Clinical symptoms depend on the size, location and
number of new lesions. Thus, we assume that the pathological process that causes
silent lesion recurrence on MRI is the same as the process that causes clinical
recurrent strokes. Magnetic resonance imaging may depict pathological changes
before the development of clinical stroke symptoms.”