We share tips about what to wear, who to date, etc, but when it comes to health, many life-saving tips go unnoticed. Here, we take time to try and shed more light on a relatively still unexplained condition, endometriosis, not be confused with endometrial cancer. Here is the difference:
While pelvic pain is a symptom of endometrial cancer, it is also one of the main symptoms of a health condition called endometriosis, which very rarely leads to endometrial cancer.
What Is Endometriosis?
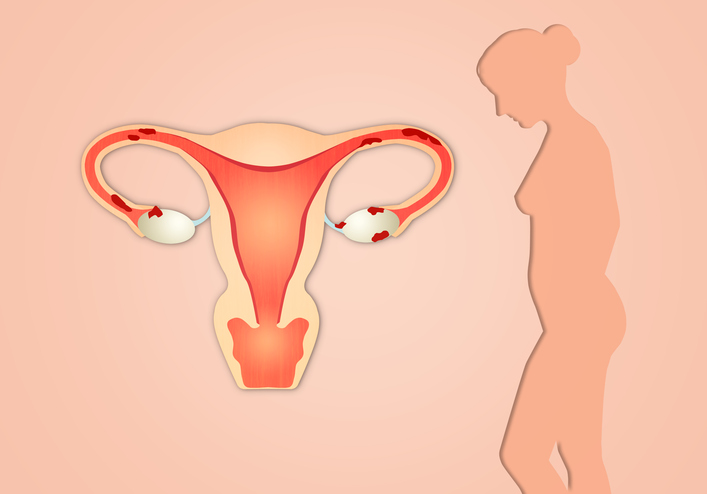
When a woman gets her period once a month, the lining of the uterus (which is called the endometrium) breaks down and is shed as menstrual flow. When a woman has endometriosis, the type of tissue that makes up the lining of the uterus also shows up in other parts of her body, including the ovaries, the fallopian tubes, the bowels, and the bladder. During her period, this tissue breaks down. But since it’s outside the uterus, it can’t leave the body during menstruation, and cysts and scar tissue may form as a result.
In even more rare cases, endometriosis has been found inside the vagina, inside the bladder, on the skin, even in the lung, spine, and brain.
In addition to causing pain that can become quite severe, endometriosis can also cause scar tissue and adhesions to develop that can distort a woman’s internal anatomy. In advanced stages, internal organs may fuse, causing a condition known as a “frozen pelvis.” It is also estimated that 30-40% of women with endometriosis may become infertile.
Currently, endometriosis affects over five million women in the United States.
What Is Endometrial Cancer?
The abnormal tissue implants that grow as a result of endometriosis aren’t cancerous. They’re simply benign tissues that grow in areas where they aren’t meant to grow. Endometriosis very rarely causes endometrial cancer or uterine cancer, as these cancers are seen in fewer than 1 percent of all women with endometriosis. In the rare instances where endometrial cancer does develop, it’s typically found in older women — often post-menopausal — and the prognosis is generally pretty positive.
When associated with any type of uterine cancer, endometriosis most commonly (but still very rarely) is found with a type called endometrioid cancer — however, research hasn’t shown that endometriosis causes this type of cancer.
Even though endometriosis rarely leads to endometrial cancer, these benign growths can still cause serious problems and pain.
Each month, a woman’s body releases hormones that signal the start of the menstrual period, when the endometrium sheds its








