"I'm the most doctor-tested man alive."
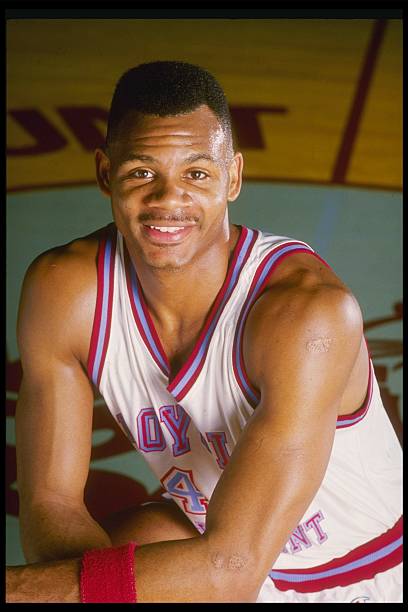
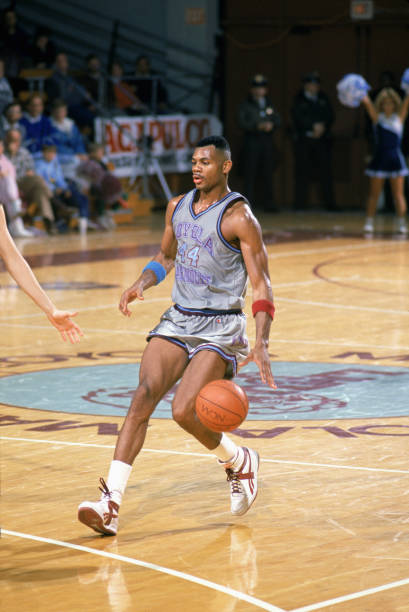
Eric Wilson "Hank" Gathers Jr. was an American college basketball player for the Loyola Marymount Lions in the West Coast Conference. As a junior in 1989, he became the second player in NCAA Division I history to lead the nation in scoring and rebounding in the same season. This was particularly impressive since he was diagnosed with a very serious heart condition, Hypertrophic Cardiomyopathy (HCM) that required him to regularly take medication to manage.
"I feel great. I'm in the best shape of my life. My mom's out here, and I'm looking forward to some good home cooking." Gathers said at a Loyola Marymount game. He also informed a different reporter that his medication by this point was "almost down to nothing." It was later discovered that he reportedly hadn’t taken his meds that day at all. His doctors prescribed him a drug called Inderal, or propranolol. Gathers was reported to have minimized the dose because he felt sluggish while exercising. The drug belongs to a class called beta-blockers, which are often prescribed for cardiomyopathy, and sluggishness is a well-known side effect.
This decision, unfortunately, cost the promising then 23-year-old athletic star his life. During the 1990 game, he collapsed on the court and never woke up.
This left the country shaken, especially since little was known about the condition at the time.
What is hypertrophic cardiomyopathy?
According to the American Heart Association, hypertrophic cardiomyopathy is most often caused by abnormal genes in the heart muscle. These genes cause the walls of the heart chamber (left ventricle) to contract harder and become thicker than normal.
The thickened walls become stiff. This reduces the amount of blood taken in and pumped out to the body with each heartbeat.
RELATED: 8 Surprising Factors That Could Be Putting Your Heart At Risk
What are the warning signs?
The American Heart Association lists the following symptoms:
- Chest pain, especially with physical exertion
- Shortness of breath, especially with physical exertion
- Fatigue
- Arrhythmias (abnormal heart rhythms)
- Dizziness
- Lightheadedness
- Fainting (syncope)
- Swelling in the ankles, feet, legs, abdomen and veins in the neck
This is a chronic disease that can get worse over time and can lead to poorer function and quality of life, long-term complications and more financial and social burden.
People with HCM often need to make lifestyle changes, such as limiting their activity, to adjust for their disease.
As HCM progresses, it can cause other health problems. People with HCM are at higher risk for developing atrial fibrillation, which can lead to blood clots, stroke and other heart-related complications. HCM may also lead to heart failure. It can also lead to sudden cardiac arrest, but this is rare.
HCM has been cited as the most common reason for sudden cardiac death in young people and athletes under the age of 35.
- What are the treatments?
Typically medications or surgical procedures are prescribed by physicians to patients.
Beta-blockers, calcium channel blockers and diuretics offer limited and varying relief of symptoms. They may help with function but may also have adverse side effects.
Additionally, surgical procedures are recommended for particularly serious cases. The American Heart Association cites the following surgeries to help treat the condition:
Septal myectomy – Septal myectomy is open-heart surgery. It’s considered for people with obstructive HCM and severe symptoms. This surgery is generally reserved for younger patients and for people whose medications aren’t working well. A surgeon removes part of the thickened septum that’s bulging into the left ventricle. This improves blood flow within the heart and out to the body.
Alcohol septal ablation (nonsurgical procedure) – In this procedure, ethanol (a type of alcohol) is injected through a tube into the small artery that supplies blood to the area of heart muscle thickened by HCM. The alcohol causes these cells to die. The thickened tissue shrinks to a more normal size. The risks and complications of heart surgery increase with age. For this reason, ablation may be referred to myectomy in older patients with other medical conditions.
Surgically implanted devices – Surgeons can implant several types of devices to help the heart work better, including:
- Implantable cardioverter-defibrillator (ICD) – An ICD helps maintain a normal heartbeat by sending an electric shock to the heart if an irregular heartbeat is detected. This reduces the risk of sudden cardiac death.
- Pacemaker – This small device uses electrical pulses to prompt the heart to beat at a normal rate.
- Cardiac resynchronization therapy (CRT) device – This device coordinates contractions between the heart’s left and right ventricles.
Heart transplant – In HCM patients with advanced, end-stage disease, a heart transplant may be considered. In this procedure, a person’s diseased heart is replaced with a healthy donor heart.
Unfortunately, cardiomyopathy cut Hank’s life short, but due to medical advancement throughout the years, others don’t have to meet the same fate.









