According to Earvin “Magic” Johnson, his decision to endorse OraQuick, the first FDA-approved home HIV test, comes from what he knows personally about the factors endangering at-risk African American and Hispanic communities.
According to Earvin “Magic” Johnson, his decision to endorse OraQuick, the first FDA-approved home HIV test, comes from what he knows personally about the factors endangering at-risk African American and Hispanic communities.
“OraQuick is a game changer for us…especially when you think about the stigmas in the black and brown community,” Johnson said recently.
Celebrate great health! LIKE BlackDoctor.org on Facebook!
“The black and brown community…these are the people who I was thinking about most when I thought about this kit,” Johnson said. “We don’t want to go to the clinic. We don’t want anybody to see us at the doctor. We don’t want people to know if we’re HIV-positive or not.”
OraQuick delivers results in about 20 minutes in the privacy of a person’s home. Chain drugstores, including Duane Reade and CVS, carry the test for around $40.
“Now we’re saying, ‘You can have this test and you can do it in your own home, privately,'” Johnson said. “‘If you want people to be there or not, that’s up to you. You just need to know your status.’ It makes a difference, because I think more people will be willing to get tested. They’ll know their results, and if they are HIV-positive, there’s great information available that can get them to a doctor, including a 1-800 hotline. If they have questions, someone will be able to answer them.”
Magic Johnson: His Personal Mission
“When I announced 21 years ago, AIDS activist Elizabeth Glaser told me on her dying bed that I had to become the face of this disease,” Johnson said at a presentation for Orasure Technologies. He added that endorsing OraQuick is just one of the ways he’s making good on his promise to Glaser, who contracted HIV from a blood transfusion she received while giving birth in 1981.
“She felt like the disease needed a face to raise awareness levels, and she wanted me to get out and educate people,” Johnson told the crowd. “I promised her that I’d go out and do it.”
Blacks & HIV
Despite making up just 13 percent of the population, African Americans bear the brunt of the HIV/AIDS epidemic in the U.S., accounting for nearly half of the estimated 1.2 million people living with the disease, nearly half of new HIV cases, and half of annual AIDS-related deaths, according to Phil Wilson, president and CEO of the Black AIDS Institute.
Organizations like the CDC have called for routine HIV screening as a way to reduce the stigma some associate with showing up at an HIV clinic, a proposal that was also made by members of the U.S. Preventive Services Task Force earlier this year. If agreed upon, the recommendations will make HIV testing as standard a practice as checking cholesterol levels, fundamentally changing how the virus is detected and treated, according to experts.
Hispanics & HIV
According to the Centers for Disease Control, Hispanics who learn they are HIV positive progress to AIDS faster than any other racial or ethnic group. Forty-two percent of Hispanics diagnosed as HIV positive progress to AIDS within 12 months, compared to 34 percent of non-Hispanic whites and 35 percent of African-Americans.
In addition, the rate of new HIV infections among Hispanic women is more than four times that of white women and the rate of new HIV infections among Hispanic men is almost three times that of white men.
OraQuick Facts
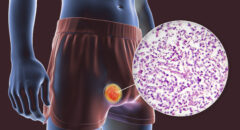
OraQuick, which received approval by the Food and Drug Administration earlier this year, produces results in 20 minutes and retails at pharmacies, such as CVS and Walgreens, and online for approximately $40. The test, which has been used by health care providers for just over a decade, uses a mouth swab to detect antibodies to HIV-1 and HIV-2 in oral fluid. While it has been put through a battery of tests itself, the FDA cautioned that the test is not 100 percent accurate in identifying people with the virus.
In a trial conducted by test maker Orasure, OraQuick detected HIV in those carrying the virus only 92 percent of the time, but was 99.9 percent accurate in ruling out HIV in patients who are not carrying the disease.
That means the test could miss 1 in 12 HIV-infected people who use it, according to the FDA, but would incorrectly identify only one patient as having HIV for every 5,000 HIV-negative people tested.
An inaccurate reading can result if a person takes the test too close to their moment of incidence rather than after three to six months, the approximate time HIV takes to appear in the human body, experts say.