
Hidden blood clot symptoms often involve subtle or “silent” signs, as deep vein thrombosis (DVT) in the legs can be unnoticed or cause dull pain, tenderness, swelling, and warmth. Symptoms are more obvious when a clot travels to the lungs, causing sudden shortness of breath, chest pain, or a fast heartbeat, which require immediate medical attention.
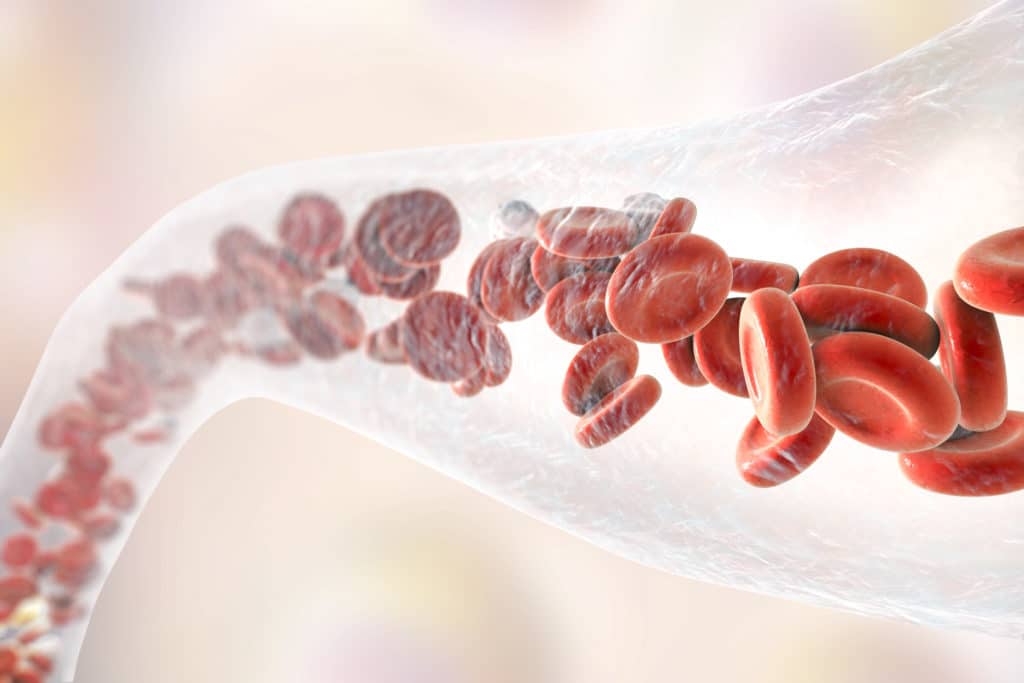
DVT typically forms deep within a vein in the leg. When a blood clot forms, it can obstruct blood flow, leading to uncomfortable symptoms. If a clot breaks free from the spot where it formed, it may cause a potentially life-threatening condition known as pulmonary embolism, when the clot travels through blood vessels and enters the lung.
Not all blood clots in the leg lead to pulmonary embolism; some resolve on their own. But if you notice signs that you may have DVT, seeing a doctor quickly may help you avoid dangerous complications.
These veins are invisible to us, so a clot could be “silent” without causing any symptoms.
What Causes Blood Clots?
Blood clots happen because substances in your blood become thick and form a semi-solid mass. This process helps heal injuries, but it can be dangerous if clots appear without reason or break free.
Lack of movement or long travel
Your blood slows down during periods of stillness. Long hours of sitting at a desk or during travel substantially increase your chances of developing clots. Research shows that staying immobile for more than 3 days puts hospitalized patients at risk for proximal deep vein thrombosis (DVT). The risk becomes 5 times higher with temporary immobilization. This highlights why understanding how to prevent blood clots is important, especially for travelers or those on bed rest.
Surgery or injury
Blood clots often develop after surgery and physical trauma. The risks are higher with major operations, especially those that involve your abdomen, pelvis, hip, or legs. About 40% of post-surgery blood clots occur in the hospital, and 60% develop within 90 days after patients go home. Recent hospital stays or surgeries are linked to more than half of all blood clots first spotted in outpatient settings.
Medical conditions and medications
These health conditions raise your blood clotting risk:
- Cancer (one of the most common causes)
- Heart conditions (arrhythmia, heart attack, heart failure)
- Obesity
- Inflammatory diseases
- COVID-19
- Diabetes and high blood pressure
- Birth control pills and hormone replacement therapy that contain estrogen can increase your risk of blood clots. Pregnancy also boosts clotting factors to manage expected bleeding.
Family history and genetics
Your risk of venous thrombosis doubles with a family history and quadruples if multiple relatives have had clots. Common inherited clotting disorders include Factor V Leiden mutation (found in 5% of people with European ancestry) and Prothrombin G20210A mutation (present in 2% of people).
The danger grows much higher with multiple risk factors. People who have both genetic and environmental risk factors plus a family history face a risk 64 times higher than those without any risk factors.
Hidden Blood Clot Signs You Shouldn’t Ignore
5. Skin Color
If a clot plugs up veins in your arms or legs, they may look bluish or reddish. Your skin also might stay discolored from the damage to blood vessels afterward. A pulmonary embolism (PE) in your lung could make your skin pale, bluish, and clammy.
Red blood cells provide oxygen to body tissues. Most of the time, nearly all red blood cells in the arteries carry a full supply of oxygen. These blood cells are bright red and the skin is pinkish or red.
Blood that has lost its oxygen is dark bluish-red. People whose blood is low in oxygen tend to have a bluish color to their skin. This condition is called cyanosis.
Depending on the cause, cyanosis may develop suddenly, along with shortness of breath and other symptoms.
Cyanosis that is caused by long-term heart or lung problems may develop slowly. Symptoms may be present, but are often not severe.
When the oxygen level has dropped only a small amount, cyanosis may be hard to detect.
In dark-skinned people, cyanosis may be easier to see in the mucous membranes (lips, gums, around the eyes) and nailbeds.
4. Swelling
Most people typically have some degree of leg swelling at a point in their lives, especially near the end of the day. That’s not the swelling we worry about. Instead, watch for swelling that:
- Occurs suddenly or more dramatically than usual.
- Lingers throughout the day.
- Doesn’t get better with leg elevation.
Edema, or swelling, can become an emergency when it is accompanied by the following symptoms:
- Sudden onset: Swelling that develops rapidly without an obvious cause.
- Severe pain: Pain that is intense or unbearable.
- Shortness of breath: Difficulty breathing or wheezing.
- Chest pain: Pain in the chest that may radiate to the arm or back.
- Confusion or dizziness: Mental changes that may indicate a serious underlying condition.
- Fever: A high temperature that may indicate an infection.
- Coughing up blood: This could be a sign of a blood clot in the lungs.
- One-sided swelling: Swelling that is only present on one side of the body.
- Swelling that worsens despite home treatment: If the swelling does not improve with elevation, rest, or compression stockings.
3. Pain in Your Leg
New leg pain — like a pain in your calves, a charley horse, or something you would consider as “growing pains” — could signal a blood clot in the leg. But if the pain only lasts for a few seconds and doesn’t come back, it’s probably not a blood clot.
Blood clot symptoms don’t come and go quickly. So if your pain doesn’t go away after your allotted time or it changes in the type of pain you’re used it, it would be good to talk to your doctor about the length of time and the type of pain you have.
Also, if you feel a lump or cord that is tender to the touch can be caused by clots in superficial veins outside the muscle.
2. Irregular Heartbeat
Does your heartbeat seem to be off? Does it feel like it beating too fast? An irregular heartbeat, especially atrial fibrillation (AFib), can lead to blood clots because of sluggish blood flow in the heart’s upper chambers, which increases the risk of serious complications like stroke, pulmonary embolism, or organ damage. Symptoms of a blood clot include numbness, weakness, or paralysis, especially on one side of the body, as well as trouble with speech, walking, or coordination. If you suspect an irregular heartbeat or symptoms of a blood clot or stroke, you should seek emergency medical care immediately.
How AFib Causes Blood Clots
- Stagnant Blood Flow:
In atrial fibrillation (AFib), the heart’s two upper chambers (the atria) quiver instead of contracting effectively. - Clot Formation:
This ineffective pumping causes blood to pool in the atria, creating a stagnant environment where blood clots can form. - Embolism Risk:
If a blood clot detaches from the heart, it’s called an embolus. This embolus can travel through the bloodstream and block blood flow to vital organs, particularly the brain, causing a stroke.
1. Changing in Your Breathing
While changing in your breathing doesn’t sound too bad, it can be very troublesome when it comes to a blood clot.
If you feel that something may be off, be aware of breathing changes like:
- Shortness of breath: that may be sudden or worsen with exertion
- Rapid breathing
- Coughing, sometimes with bloody mucus
- Wheezing
Shortness of breath and difficulty breathing are common symptoms related to a number of issues. But it is important to recognize that although a symptom may seem minor, it could be the tip of the iceberg.
How Long Before a Blood Clot Can Take Your Life?
The time frame before a pulmonary embolism (PE) becomes fatal varies depending on the severity of the embolism and the patient’s overall health.
Immediate death:
In some cases, a large PE can block a major blood vessel in the lungs immediately, leading to sudden death. This occurs in about 25% of cases.
Within hours or days:
If the PE is not treated promptly, it can cause significant damage to the heart and lungs. Death may occur within hours or days in these cases.
Within weeks or months:
Smaller PEs or those that are treated early may take weeks or months to become fatal. The risk of death is higher if the patient has underlying heart or lung conditions.
According to the National Heart, Lung, and Blood Institute, the mortality rate for PE is:
30-day mortality: 10-15%
1-year mortality: 20-25%
It’s important to note that these are just estimates, and the actual time frame may be different for each individual patient. If you suspect you have a PE, seek immediate medical attention as it is a life-threatening condition.









