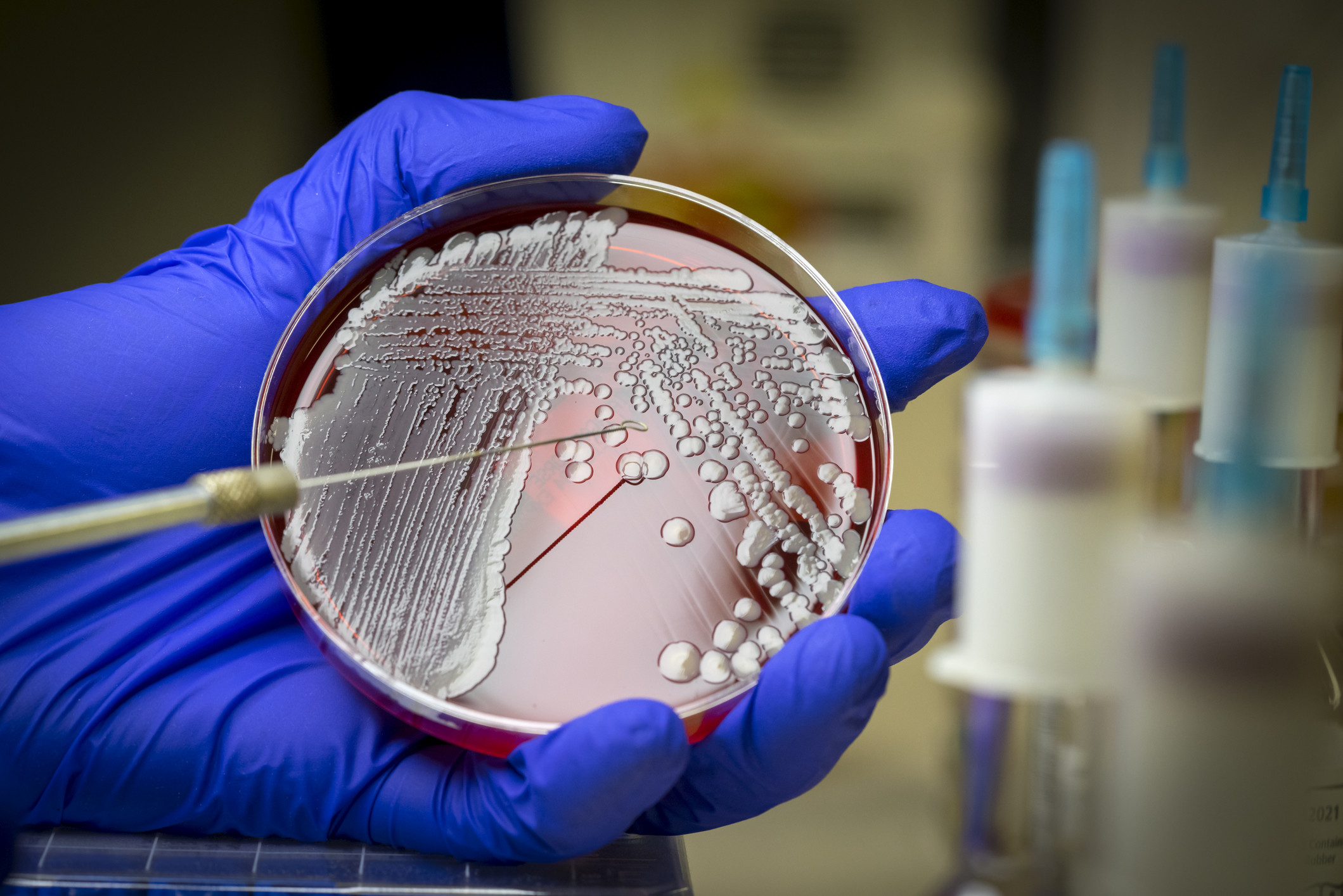
Drug-resistant superbugs are killing more than 35,000 Americans each year, averaging one death every 15 minutes, according to a new report from the Centers for Disease Control and Prevention (CDC).
On November 13, the CDC issued its 2019 Antibiotic Resistance Threats in the United States report, underscoring the major health threats posed by bacterial and fungal infections that are resistant to treatment with antibiotics. According to the report, these superbugs are responsible for more than 2.8 million infections in this country annually, or a new infection every 11 seconds.
A superbug is a term coined by the media to describe bacteria that cannot be killed using multiple antibiotics.
"What the public should know is that the more antibiotics you’ve taken, the higher your superbug risk," says Eric Biondi, MD, who runs a program to decrease unnecessary antibiotic use. "The more encounters you have with the hospital setting, the higher your superbug risk."
"Superbugs should be a concern to everyone," Coombes says. "Antibiotics are the foundation on which all modern medicine rests. Cancer chemotherapy, organ transplants, surgeries, and childbirth all rely on antibiotics to prevent infections. If you can't treat those, then we lose the medical advances we have made in the last 50 years."
The CDC also added two new germs to the urgent category: Drug-resistant Candida auris and carbapenem-resistant Acinetobacter.
“Candida auris is a new species that presented in the last couple of years,” says M. Valeria Fabre, MD, an assistant professor of medicine and an infectious-disease expert at Johns Hopkins University School of Medicine in Baltimore. “It’s a highly resistant yeast that causes...
...invasive infections, such as a bloodstream infection. These are very serious infections, and they’re very resistant to the antifungal treatments that we have,” she says.
This bug is typically associated with healthcare settings, such as long-term care facilities. “Elderly people can be at high risk for getting this infection,” Dr. Fabre says.
Carbapenem-resistant Acinetobacter is the kind of bacteria that’s really driving antibiotic resistance around the world, according to Fabre.
“The term ‘carbapenem-resistant’ is a red flag,” she says. Carbapenems are a class of very effective antibiotic agents. “We usually reserve these medicines for the most resistant infections, so we are talking about an infection that is resistant to this ‘big gun’ antibiotic,” she says.
“It’s very commonly seen in patients who require respiratory support in the hospital,” Fabre says. “Patients who get this kind of infection have a very high risk of death.”
The three other urgent threats on the CDC list are:
- Clostridioides difficile (C. diff), a bacteria that can cause life-threatening diarrhea and colitis (inflammation of the colon)
- Carbapenem-resistant Enterobacteriaceae, also known as "nightmare bacteria," which are resistant to nearly all antibiotics
- Drug-resistant Neisseria gonorrhoeae, which causes the sexually transmitted disease gonorrhea.