Ovarian cancer is often referred to as the “silent killer” because its symptoms can be subtle and easily mistaken for common digestive or menstrual issues. However, for Black women, the silence surrounding this disease is compounded by a loud and persistent disparity in healthcare outcomes.
Although Black women have a lower incidence rate of ovarian cancer, they unfortunately experience significantly worse survival rates compared to other populations. While there has been a modest improvement in survival rates among Caucasian women over the last four decades, there has been no such progress observed for Black women, highlighting a concerning disparity.
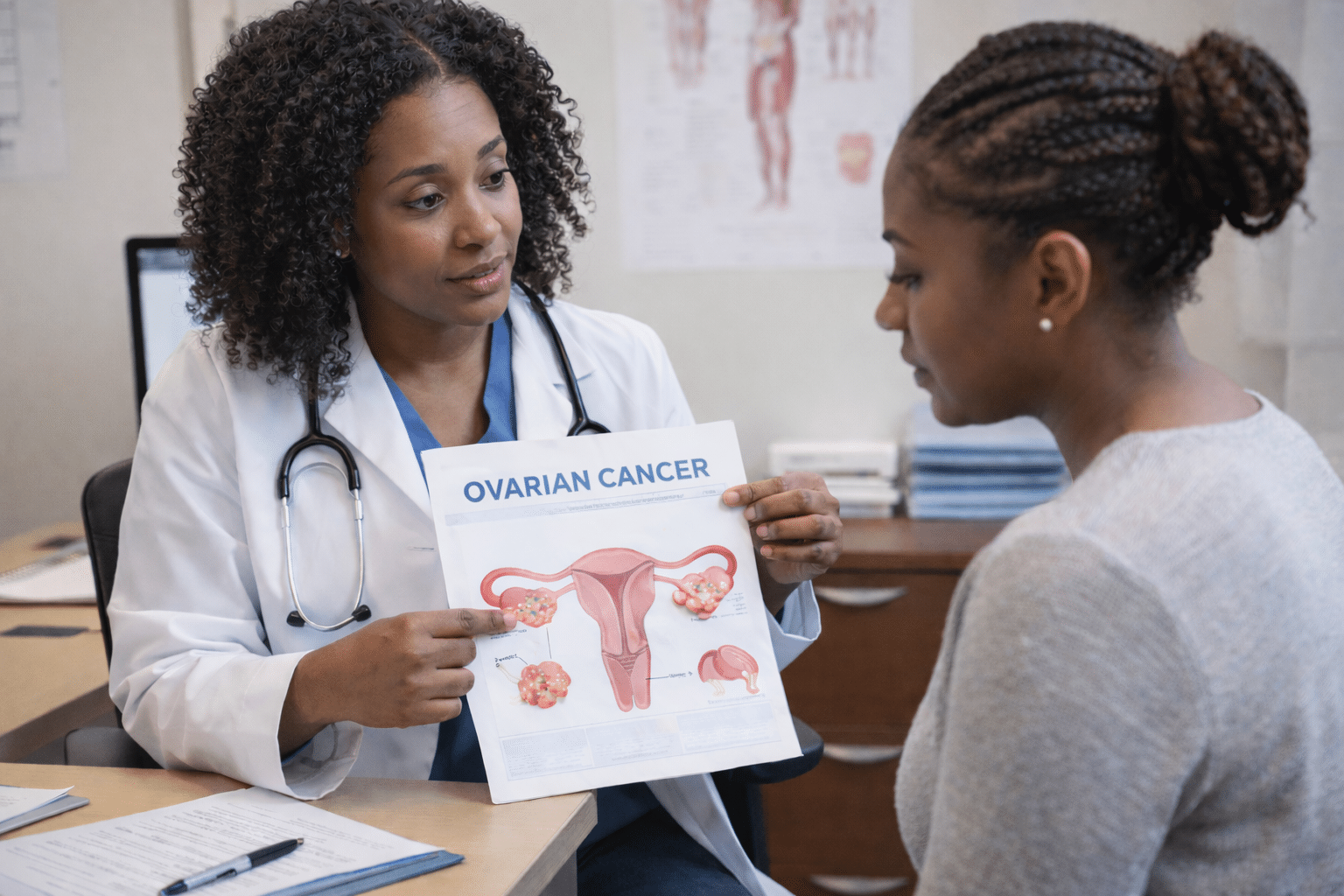
The exact reasons behind this substantial difference in ovarian cancer development and survival outcomes between Black American women and Caucasian women remain elusive and require further investigation. However, it is essential to acknowledge that educating women about ovarian cancer and its implications, while simultaneously encouraging open and effective communication between patients and their healthcare providers, represents a necessary first step in addressing this health inequity and improving outcomes for all women.
What Is Ovarian Cancer?
This cancer originates in the ovaries, which are responsible for producing a woman’s eggs and are the primary source of the female hormones estrogen and progesterone. Recent advancements in ovarian cancer treatments have shown improved effectiveness, and the most promising outcomes are observed when the disease is detected at an early stage.
RELATED: 5 Ways to Decrease Ovarian Cancer Risk
So, What Are The Symptoms?
Because the ovaries are located deep within the pelvic cavity, tumors can grow quite large before they cause noticeable pain. The symptoms of ovarian cancer are often vague, which is why it is vital to listen to your body.
Symptoms include:
- Bloating or pressure in the belly
- Pain in the abdomen or pelvis
- Feeling full too quickly during meals
- Urinating more frequently
While these symptoms are often caused by non-cancerous conditions (like IBS or fibroids), the key is persistence. If you experience these symptoms daily for more than two to three weeks, it is time to schedule a consultation with your healthcare provider.
Know Your Family History
A family history of cancer, particularly ovarian, breast, or colon cancer, can significantly increase a woman’s risk of developing ovarian cancer. Research indicates that inherited genetic alterations are responsible for approximately 10 percent of ovarian cancers. These genetic changes can include mutations in the BRCA1 and BRCA2 genes, which are also associated with breast cancer. Women with a strong family history of these cancers are encouraged to discuss the possibility of increased risk and potential preventative measures with their healthcare providers.
Age Isn’t Just A Number
Age is the most significant risk factor for ovarian cancer. The likelihood of developing the disease increases after a woman experiences menopause. Furthermore, postmenopausal hormone therapy might elevate the risk. The connection appears most pronounced in women who take estrogen without progesterone for a period of five to 10 years. However, medical professionals are unsure if taking a combination of estrogen and progesterone also increases the risk.
READ: Fibroid Pain: Tips For Managing Your Sex Life
Obesity & Ovarian Cancer
Studies show that obesity significantly increases a woman’s risk of developing ovarian cancer compared to women who are not obese. Furthermore, the mortality rates for ovarian cancer are also higher among obese women. The risk appears to be directly correlated with body weight, with heavier women facing the greatest danger.
Ovarian Cancer Screening Tests
There are two ways to screen for ovarian cancer before it causes symptoms or shows up during a routine gynecologic exam. One is a blood test for elevated levels of a protein called CA-125. The other is an ultrasound of the ovaries. Unfortunately, neither technique has been shown to save lives when used in women of average risk. For this reason, screening is only recommended for women with strong risk factors.
Ovarian Cancer Survival Rates
Ovarian cancer can be a frightening diagnosis, with five-year relative survival rates ranging from 89 to 18 percent for epithelial ovarian cancer, depending on the stage at diagnosis. It’s important to note that these figures are based on data from women diagnosed between 1988 and 2001. Given advancements in treatment, the outlook for those diagnosed today may be even more positive. For LMP tumors, the five-year relative survival rates range from 99 to 77 percent.
The disparity in ovarian cancer survival for Black women is a call to action. Education is the first step in dismantling this health inequity. By understanding the symptoms, knowing your family history, and insisting on thorough evaluations from healthcare providers, you can take control of your health.
If you feel your concerns are being dismissed, do not hesitate to seek a second opinion or ask for a referral to a gynecologic oncologist. These specialists are specifically trained to manage ovarian cancer and are linked to better survival outcomes for patients.
RELATED: Genetic Testing & Ovarian Cancer: What Black Women Need to Know
When To See A Doctor: The “Two-Week Rule”
Knowing the symptoms is only half the battle; knowing when they transition from a nuisance to a medical priority is life-saving. Because these symptoms mimic common issues like Irritable Bowel Syndrome (IBS) or PMS, many women wait too long to seek help.
You should schedule an appointment if:
-
Frequency: You experience one or more of the symptoms listed above more than 12 times in a single month.
-
Duration: The symptoms persist daily for two weeks or longer despite changes in diet or over-the-counter treatments.
-
New Onset: These are symptoms that are not “normal” for you and have started recently (within the last six months).
Pro-Tip: Keep a “Symptom Diary.” Write down what you feel, how long it lasts, and how many times it occurs per week. Bringing this log to your doctor provides concrete evidence that your concerns aren’t just “in your head” or “related to stress.”









