
A diagnosis of heart failure can be devastating, especially for someone who has been physically active and seemingly in otherwise good health. While there are many reasons why someone could develop heart failure, such as coronary artery disease or high blood pressure, there is another possible cause that often goes overlooked.
Have you heard of transthyretin amyloid cardiomyopathy, also known as ATTR-CM? Chances are you haven’t. This rare, life-threatening condition is a type of cardiac amyloidosis and often goes undiagnosed, as its symptoms can mimic more common causes of heart failure or even seem completely unrelated to a heart condition.1-3 ATTR-CM occurs when transthyretin, a transport protein that naturally circulates in the blood, becomes unstable, dissociates, and misfolds. The misfolded protein can aggregate and form amyloid fibrils that build up in the heart and other parts of the body as amyloid deposits, which over time, can cause the heart muscle to become stiff, eventually resulting in heart failure.4
There are two forms of ATTR-CM, hereditary or variant (hATTR) and wild-type (wtATTR). The hereditary form of the disease is caused by a mutation in the transthyretin gene. It can occur in people as early as their 50s-60s and one such mutation, called V122i, almost exclusively affects those of African, African American or Afro-Caribbean descent. The wild type form, which is thought to be more common and is not caused by a mutation, usually affects men after age 60.1-8
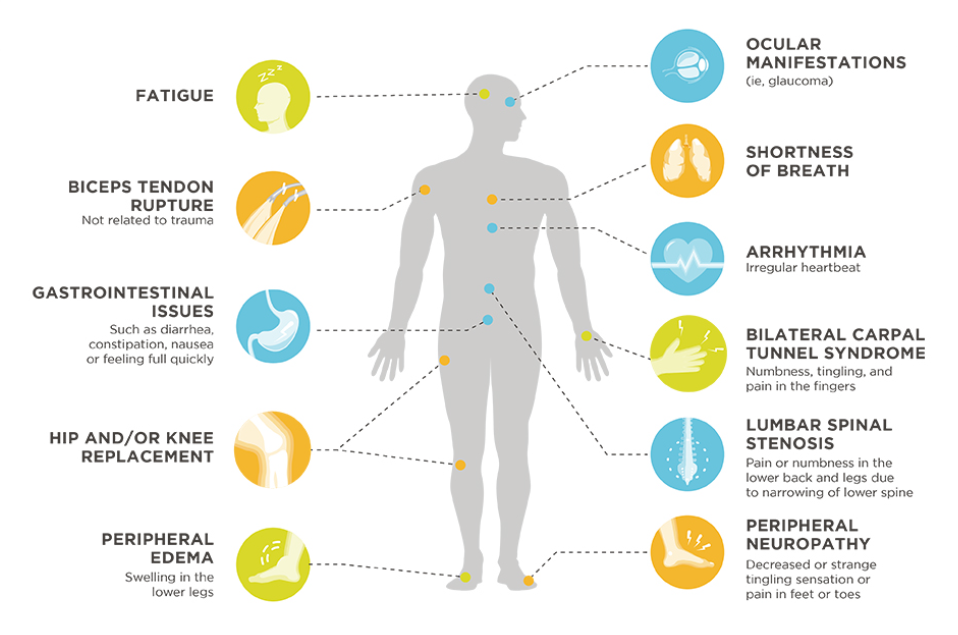
Some heart failure symptoms that may also be related to ATTR-CM include shortness of breath, fatigue, swelling of the ankles, and irregular heartbeat (eg, arrhythmia). Additionally, amyloid can build up in other areas in the body, not just the heart, leading to other seemingly unrelated signs and symptoms such as carpal tunnel syndrome; GI problems such as diarrhea, constipation or nausea; and pain or numbness in the lower back or legs. Patients with heart failure may also experience an intolerance to standard heart failure therapies, which could be a sign of ATTR-CM.9-14
Awareness of ATTR-CM is low within the physician community, which also may contribute to underdiagnosis of the disease. For this reason, it’s important for heart failure patients or their caregivers to talk to a cardiologist to confirm or rule out the disease if the symptoms of ATTR-CM sound familiar.
As part of the diagnostic process, a cardiologist may order an electrocardiogram (ECG) or cardiac imaging such as an echocardiogram or cardiac MRI to assess how the heart is working and look for signs that may suggest ATTR-CM.15,16 Once ATTR-CM is suspected, a cardiologist can perform several tests to help diagnose the disease. This may include nuclear scintigraphy and/or a cardiac biopsy. If a diagnosis of ATTR-CM is made, genetic testing and counseling may be suggested to rule out the hereditary form of ATTR-CM, which can have implications for the patient as well as their family members.15
With the disproportionate rates of heart failure, heart attacks, and other serious heart conditions in the Black community, it’s important to fully explore the underlying cause of these conditions with the help of a cardiologist. Always be sure to share as much information as possible with your doctor, which can help guide you on the right path for diagnosis. To learn more about ATTR-CM and access other resources on the disease, visit YourHeartsMessage.com.17,18
____________________________________________________________________________
Sipe JD, Benson MD, Buxbauym JN, et al. Amyloid fibril proteins and amyloidosis: chemical identification and
clinical classification. Amyloid. 2016;23(4): 209-213.
2 Connors LH, Sam F, Skinner M, et al. Heart failure due to age-related cardiac amyloid disease associated with wild-type transthyretin: a prospective, observational cohort study. Circulation. 2016;133(3):282-290.
3 Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C. Addressing common questions encountered in the
diagnosis and management of cardiac amyloidosis. Circulation. 2017;135(14):1357-1377.
4 Siddiqi OK, Ruberg FL. Cardiac amyloidosis: an update on pathophysiology, diagnosis and treatment. Trends in Cardiovascular Medicine. 2017;1050-1738.
5 González-López E, Gallego-Delgado M, Guzzo-Merello G, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J. 2015;36(38):2585-2594.
6 Mohammed SF, Mirzoyev SA, Edwards WD, et al. Left ventricular amyloid deposition in patients with heart failure and preserved ejection fraction. JACC Heart Fail. 2014;2(2):113-122.
7 Swiecicki PL, Zhen DB, Mauermann ML, et al. Hereditary ATTR amyloidosis: a single-institution experience with 266 patients. Amyloid. 2015;22(2):123-131.
8 Ruberg FL, Berk JL. Transthyretin (TTR) cardiac amyloidosis. Circulation. 2012;126(10):1286-1300.
9 Nativi-Nicolau J, Maurer MS. Amyloidosis cardiomyopathy: update in the diagnosis and treatment of the most common types. Curr Opin Cardiol. 2018;33(5):571-579.
10 Maurer MS, Hanna M, Grogan M, et al. Genotype and phenotype of transthyretin cardiac amyloidosis: THAOS
(Transthyretin Amyloid Outcome Survey). J Am Coll Cardiol. 2016;68(2):161-172.
1 Bishop E, Brown EE, Fajardo J, et al. Seven factors predict a delayed diagnosis of cardiac amyloidosis. Amyloid. 2018; doi.10.1080/13506129.2018.1498782.
2 Narotsky DL, Castaño A, Weinsaft JW, Bokhari S, Maurer MS. Wild-type transthyretin cardiac amyloidosis: novel insights from advanced imaging. Can J Cardiol. 2016;32(9):1166.e1-1166.e10.
3 Brunjes DL, Castano A, Clemons A, Rubin J, Maurer MS. Transthyretin cardiac amyloidosis in older Americans. J Card Fail. 2016;22(12):996-1003.
4 Castaño A, Drachman BM, Judge D, Maurer MS. Natural history and therapy of TTR-cardiac amyloidosis: emerging disease modifying therapies from organ transplantation to stabilizer and silencer drugs. Heart Fail
Rev. 2015;20(2):163-178.
5 Gillmore JD, Maurer MS, Falk RH, et al. Non-biopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016;133(24):2404-2412.PP-R1D-USA-0493
6 Nativi-Nicolau J, Maurer MS. Amyloidosis cardiomyopathy: update in the diagnosis and treatment of the most common types. Curr Opin Cardiol. 2018;33(5):571-579.
7 Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–245.doi:10.2174/1573403X11666141122220003.
8 Bonow RO, Grant AO, Jacobs AK. The cardiovascular state of the union: confronting healthcare disparities. Circulation 2005; 111(10): 1205-7.







