
We’ve all experienced the throbbing, distracting discomfort of a headache. Headaches vary. Everybody gets headaches. Types of headaches differ in cause, duration, and severity.
Most Common Primary Types of Headaches
Primary headaches typically involve head pain. Your headache isn’t going to be caused by illness or allergies.
These headaches can be episodic or chronic:
- Episodic headaches may occur up to 15 times a month. They might last 30 minutes to hours.
- Chronic headaches recur. More than 15 days every month. Pain treatment is needed in these circumstances.
Tension headache
Tension headaches cause a dull, agonizing pain across the head. Non-throbbing. Neck, forehead, scalp, or shoulder muscles may be irritated. Tension headaches are common, as stress causes them.
Cluster headache
Cluster headaches are sharp and searing. They appear around, behind, or on one side of one eye. Signs include:
- swelling, redness, flushing, and sweating on the side that’s affected by the headache
- nasal congestion and eye tearing on the same side as the headache
Multiple headaches develop. Every headache lasts 15 minutes to 3 hours. Cluster headaches cause one to four headaches a day, generally simultaneously. Another headache shortly follows. Cluster headaches may last months. Symptom-free months separate clusters. Spring and autumn are cluster headache seasons. Men get them at three times the rate of women. Doctors don’t understand cluster headaches well.
Migraine
Migraine pain pulses deeply in the brain, creating daylong discomfort. Migraine symptoms hinder regular tasks. You get throbbing, one-sided migraine discomfort, light and sound sensitivity, and possibly other symptoms, including nausea and vomiting.
Visual problems may precede migraines; this is called a migraine aura. Auras can also include tingling on one side of your face or in one arm and trouble speaking. One-third of people encounter these symptoms before headaches.
- flashing lights
- shimmering lights
- zigzag lines
- stars
- blind spots
Hemicrania continua
Hemicrania continua is a mild, one-sided headache that lasts three months. It causes 1% of headaches with women having double the risk, according to researchers. Several times a day, you may sense greater intensity.
This headache may cause:
- tearing or eye redness
- nasal congestion or runny nose
- eyelid drooping
- forehead sweating
- miosis
- restlessness or agitation
Ice pick headache
Primary stabbing, or ice pick headaches, are brief, sharp head sensations. These headaches might be frequent and sudden. Ice pick headaches may be single or many stabs migrating about the head. If in the same location, this may indicate an underlying problem.
Thunderclap headache
Thunderclap headaches are intense headaches that peak in under a minute. It might be innocuous or indicate a severe disease needing medical treatment. Thunderclap headaches may signal:
- blood vessel tears, ruptures, or blockages
- stroke
- brain injury
- Reversible Cerebral Vasoconstriction Syndrome (RCVS)
- vasculitis (inflammation of blood vessels)
- pituitary apoplexy (bleeding into or loss of blood from an organ)
First-time thunderclap headache sufferers should seek medical help. If another ailment doesn’t cause your headache, you may consider therapy for future thunderclap headaches.

Most Common Secondary Types of Headaches
Another condition causes secondary headaches. Chronic headaches might result from a recurring secondary headache cause. Treating the source relieves headaches.
Allergy or sinus headache
An allergy may cause headaches. These headaches generally cause nasal and frontal discomfort. The American Migraine Foundation says 90% of “sinus headaches” are migraine. Chronic allergies or sinusitis might cause these headaches.
Hormone headache
Women often get hormonal headaches. Menstruation, birth control medications, and pregnancy influence estrogen levels, causing headaches. Menstrual migraines are headaches that may happen before, during, and after your menstruation and ovulation.
Caffeine headache
Caffeine impacts cerebral blood flow. Too much caffeine may cause headaches, as does stopping “cold turkey.” When your brain is habituated to coffee, a stimulant, you may develop a headache without it. Caffeine may affect brain chemistry, causing withdrawal headaches.
Exertion headache
After strenuous exercise, headaches develop quickly. Weightlifting, running, and sexual activity cause exertion headaches. These activities may increase blood flow to your skull, causing throbbing headaches on both sides. A headache from strenuous activity shouldn’t linger. This headache generally lasts minutes or hours.
Hypertension headache
Hypertension causes headaches, and this is serious. Dangerously high blood pressure commonly affects both sides of the head, worsening with exercise and causing a pulsation.
Rebound headache
Rebound headaches, sometimes called pharmaceutical overuse, may be dull, tension-type, or migraine-like. If you routinely use OTC pain medicines, you may be more vulnerable. Overusing these drugs increases headaches. When OTC drugs are taken more than 15 days per month, rebound headaches are likely. These over-the-counter medications:
- acetaminophen
- ibuprofen
- aspirin
- naproxen
Post-traumatic headache
Head injuries may cause post-traumatic headaches. These headaches feel similar to a migraine or stress headaches. They last 6-12 months following damage.
Spinal headache
Low cerebrospinal fluid pressure after a lumbar puncture causes a spinal headache. Postdural puncture headaches are similar. This headache might be in your:
- forehead
- temples
- upper neck
- back of the head
10 to 40% of lumbar punctures cause spinal headaches, according to research. Symptoms typically appear within 2 to 3 days but may take months. Spinal headache symptoms include:
- nausea
- neck pain
- dizziness
- visual changes
- tinnitus
- hearing loss
- radiating pain in the arms

When To See A Doctor
Some headaches need emergency medical intervention. If you have any of these symptoms with your headache, get medical attention immediately:
- stiff neck
- rash
- the worst headache you’ve ever had
- vomiting
- confusion
- slurred speech
- fever of 100.4°F (38°C) or higher
- paralysis in any part of your body
- visual loss
RELATED: Why Magnesium is so Important for Migraine Prevention
Diagnosing A Headache & Treatment
There are several ways to diagnose headaches, as there are different varieties. To treat your headache effectively, you must determine whether it’s primary or secondary. Physical exams and medical history are used to diagnose headaches. Each headache should include:
- duration
- intensity
- location
- possible triggers
Your PCP may refer you to a neurologist. Some headaches may need testing to pinpoint the reason. This includes:
- MRI or CT scan
- lumbar puncture
- blood tests
Headaches are treated differently. Not everyone responds to the same headache remedies. Treatments vary from dietary changes to invasive treatments. If you can’t treat your headaches, see a doctor.
Tension headache
An OTC pain medication may cure your occasional headache. These painkillers include:
- aspirin
- ibuprofen (Advil)
- naproxen (Aleve)
- acetaminophen and caffeine
If OTC isn’t working out, your doctor may recommend prescription medication, such as:
- indomethacin
- meloxicam (Mobic)
- ketorolac
Cluster headache
A doctor may recommend these meds to provide relief for the symptoms:
- oxygen therapy
- sumatriptan (Imitrex)
- local anesthetic (lidocaine)
Your doctor will establish a preventative strategy after a diagnosis. The following may reduce cluster headaches:
- corticosteroids
- melatonin
- topiramate (Topamax)
- calcium channel blockers
Migraine
Triptans may be used if OTC pain medications don’t treat migraine discomfort. Triptans reduce brain inflammation and blood flow. Sprays, tablets, and injections are available. Options:
- sumatriptan (Imitrex)
- rizatriptan (Maxalt, Axert)
Consult a doctor about daily migraine medication if you have:
- debilitating more than three days a month
- somewhat debilitating four days a month
- lasting longer than six days a month
Preventive migraine meds include:
- propranolol (Inderal)
- metoprolol (Toprol)
- topiramate (Topamax)
- amitriptyline
Hemicrania continua
Hemicrania continua have a complete response to NSAID indomethacin. Low doses three times daily with meals ease symptoms in 24 hours. Indomethacin may have adverse effects, particularly at large dosages, taking the lowest adequate amount.
Ice pick headache
Preventive interventions may lower the frequency or severity of future headaches. Included are:
- indomethacin
- gabapentin
- cyclooxygenase-2 (COX-2) inhibitors
- melatonin
- external hand warming
Thunderclap headache
If another ailment causes your thunderclap headache, address that issue. Primary thunderclap headaches are produced by nothing else. NSAIDs like indomethacin may help. Other therapies include:
- calcium channel blockers
- beta-blockers
- topiramate
- lithium
- triptans
Allergy or sinus headache
Mucus buildup causes sinus pressure and headaches. Examples:
- Nasal steroid sprays
- OTC decongestants like phenylephrine (Sudafed PE)
- antihistamines like cetirizine
A sinus infection might cause a headache. In such circumstances, your doctor may prescribe medicines to remove the infection and reduce your symptoms.
Hormone headache
Pain treatments like naproxen (Aleve) or frovatriptan (Frova) may help. Alternative medicines may reduce headaches each month. Helpful hints:
- relaxation techniques
- yoga
- acupuncture
- eating a modified diet
Caffeine headache
Caffeine headaches may be prevented by limiting or discontinuing caffeine.
Exertion headache
OTC pain medications like aspirin or ibuprofen (Advil) usually help. If you have exertion headaches, visit a doctor. In certain situations, they may signal a severe illness.
Hypertension headache
After blood pressure is controlled, these headaches usually disappear. As long as hypertension is controlled, they shouldn’t return.
Rebound headache
Wean yourself off pain medication to combat rebound headaches. The discomfort may aggravate initially but should lessen after a few days.
Post-traumatic headache
Doctors regularly prescribe these headache medications:
- triptans
- sumatriptan (Imitrex)
- beta-blockers
- amitriptyline
Spinal headache
Pain medications and fluids are often prescribed for spinal headaches. Avoid standing up. After a week or two, symptoms usually disappear.
Frequently Asked Questions (FAQs)
What are the most common types of headaches?
The most common types of headaches include tension headaches, migraines, and cluster headaches. These are categorized as primary headaches and are not caused by another underlying condition.
How do you know what type of headache you have?
To determine what kind of headache you have, consider the location, duration, and accompanying symptoms. Consulting a doctor for a diagnosis is recommended. Knowing your headache’s specific triggers and using a types of headaches chart can also help identify the issue.
What are the different types of headache categories?
There are two major categories: primary (e.g., migraines, tension, cluster) and secondary (e.g., sinus, hormone, post-traumatic). Each type varies in cause, intensity, and treatment method. Understanding the different types of headache helps in choosing the correct management strategy.
What are the main types of migraine headaches?
Types of migraine headaches include migraines with aura, migraines without aura, chronic migraines, and hemiplegic migraines. Each type presents unique symptoms and severity, often including visual disturbances, nausea, and one-sided head pain.
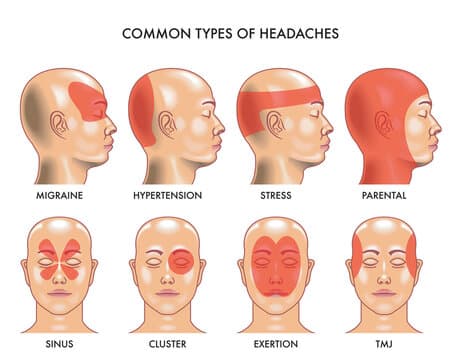
Is there a types of headaches chart I can refer to?
Yes. A types of headaches chart typically outlines pain location, duration, associated symptoms, and likely causes. It’s an excellent tool for visually comparing headache types and understanding types of headaches and causes.
What causes different types of headache pain?
The types of headaches and causes vary widely. For example, tension headaches are often due to stress, while migraines may be triggered by hormonal changes or certain foods. Cluster headaches can be seasonal, and rebound headaches stem from medication overuse.
Can headache location help diagnose the type?
Yes. Types of headaches by area—such as forehead, temples, or behind the eyes—can give clues about the headache’s origin. For example, sinus headaches affect the face, while cluster headaches concentrate around one eye.
Why is it important to identify different types of headaches?
Correctly identifying the types of headache helps in choosing effective treatments. Whether it’s avoiding triggers or selecting the right medication, knowing your headache type leads to faster relief and better management of chronic symptoms.









