Diabetes is a slow, steady illness that can turn serious very quickly. If you have diabetes, you should prepare yourself for a diabetic emergency. In a way, you're like a person living on a fault line who plans ahead for an earthquake. But you have an advantage: Instead of just preparing for a possible disaster, you can take steps to prevent it. Your doctor can tell you if you are at risk for a diabetic emergency. If you're in danger, you'll have to learn how to minimize the risks and how to respond to the worst-case scenario.
For starters, you should wear an alert bracelet or another form of I.D. that will inform medical personnel of your condition. You should also set aside a stash of extra diabetes supplies in your home in case you can't make your regular shopping trips because of a blackout, flood, blizzard, or some other unforeseen problem.
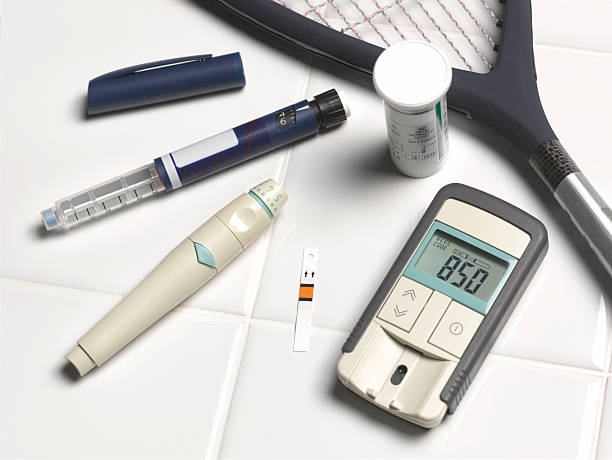
Items you may want to consider for your emergency pack include a cooler or another cold storage container with pre-made ice for keeping insulin and other supplies in case of an electrical outage; emergency glucose to treat hypoglycemia; a spare battery for your glucose test meter; canned food and several gallons of bottled water; flashlights and extra batteries; candles and matches; and, if you take insulin, extra insulin, syringes, lancets, blood test strips, and (if necessary) insulin pump supplies, according to the association Children with Diabetes.
Diabetes: 4 Things to Look For on Food Labels
Common emergencies
Extreme high blood sugar (hyperglycemia)
Read about how to prepare for the most common diabetes emergencies:
Like everyone else with diabetes, you have days when your blood sugar is a little higher than you'd like it to be. Usually, you can bring the levels back down with a little more exercise, a little less food, or a small change in medications (as directed by a doctor). If you don't follow your meal plan, if you don't take your medications, if you develop an infection or another illness, or if you are recovering from surgery or some other trauma, you may develop extremely high blood sugar, also called hyperglycemia. This is a serious illness that can damage your organs or send you into a coma.
Prepare yourself: If you're at risk for hyperglycemia -- if, for instance, you've just had a serious operation -- your doctor may recommend checking your blood sugar more often than usual. And if you've had ongoing high blood sugar, be sure to drink plenty of fluids. Ongoing hyperglycemia puts you in danger of dehydration as your body tries to eliminate the extra sugar in your body through urination. You should also know the symptoms of high blood sugar. When levels are only moderately high, some people might not have any symptoms at all. Others, however, may show one or more of the following signs:
- Unusual thirst
- Dry mouth
- Frequent urination
- Blurred vision
- Fatigue
- Weight loss
- Increased appetite
If your blood sugar climbs to dangerous levels, you may develop difficulty breathing, dizziness when standing, rapid weight loss, extreme drowsiness or confusion, or even unconsciousness. Call your doctor if your sugar levels climb too high or if you notice the symptoms above.
Prevent trouble: You can greatly reduce your risk of high blood sugar by following your meal plan and taking your medications as directed. Make sure you have a "sick day" plan for taking medications and managing your diet during an illness.
Diabetes: What to Eat When You’re Sick
Diabetic ketoacidosis (DKA)
Diabetic ketoacidosis is a life-threatening condition caused by too little insulin. Your body uses sugar for fuel, but it can't burn that fuel without the help of insulin. If you don't have enough insulin, your body is forced to burn fat instead. This is only a stopgap solution, however: When fat is broken down for energy, it releases highly acidic poisons called ketones. If ketones start collecting in your blood -- a condition called ketoacidosis -- you could face a life-threatening emergency. Patients with type 1 diabetes are especially vulnerable to ketoacidosis because they can't produce insulin on their own. Although rare, patients with type 2 diabetes who don't produce enough insulin can also develop the condition.
Prepare yourself: Test your urine for ketones anytime your blood sugar climbs to 240 or higher, the American Diabetes Association advises, or anytime you don't feel well. Make sure you have a testing kit available at all times. You may also have to check your ketones regularly if you have type 2 diabetes and low levels of insulin.
RELATED: Top 3 At-Home Diabetes Tests
If you're at risk for ketoacidosis, take the time to learn the warning signs:
- Nausea and vomiting
- Deep and rapid breaths
- A rapid heartbeat
- A fruity odor on the breath
- Abdominal tenderness
- Confusion
If your ketone levels are high or if you have symptoms of ketoacidosis, call your doctor immediately or ask someone to take you to the emergency room.
Prevent trouble: Most patients can avoid ketoacidosis by taking their insulin as directed. It's also important to get enough to eat, even if you don't have much appetite.
Hypoglycemia
If you take insulin or pills that lower blood sugar, there's a chance your blood sugar could fall too low, a condition called hypoglycemia. Hypoglycemia can occur if you overdo your insulin or medications, if you don't get enough to eat, if you burn too much sugar during exercise, or if you drink large amounts of alcohol. Hypoglycemia usually isn't fatal, but it can cause a sudden loss of consciousness -- a serious complication if you happen to be climbing some stairs or driving down the highway.
Prepare yourself: If you manage your blood sugar with insulin or drugs, be sure to check your sugar levels regularly. Your doctor can tell you how low is too low in your particular case.
If you're at risk for hypoglycemia, you and the people around you should know the symptoms of low blood sugar. If levels are just slightly below normal, you may experience one or more of these conditions:
- You may feel hungry or shaky.
- Your heart may start pounding.
- You may start to sweat or tremble.
- If your sugar drops even further, you may become confused, weak, disoriented, and combative; you may have seizures or fall into a coma.
Recognizing the warning signs can help you avoid an emergency, but only if you're prepared. Anyone at risk for hypoglycemia should always carry some hard candy, juice, sugar tablets, or some other instantly available source of sugar. Instruct your friends and family to give you something sweet (such as three to five pieces of hard candy, two or three packets of sugar, or half a cup of fruit juice) if you're still conscious but too confused or disoriented to help yourself. If you don't respond within 15 minutes, they should give you more sugar and take you to the hospital.
If you pass out from hypoglycemia, it's too late for candy. Somebody will have to give you a shot of glucagon, a hormone that will quickly raise your blood sugar. You should always have a syringe of glucagon nearby, and make sure the people around you know how to find it and how to use it.
Prevent trouble: Take your insulin or other medications as prescribed by your doctor, stick to your meal plan -- even if you don't feel like eating -- and drink alcohol only in moderation, if at all. If you exercise regularly -- an excellent idea for anyone with diabetes -- ask your doctor or exercise physiologist if you need to change your medications or diet to support your active body.
Foot sores
A cut, blister, or open sore on a foot may not seem like an emergency to most people. But if your diabetes has slowed circulation to your feet or caused nerve damage, a seemingly trivial injury can turn serious very quickly. If not treated promptly, a small sore can become infected, and in some cases, the foot may have to be amputated.
Prepare yourself: Ask your doctor if you're at risk for foot problems. If you are, learn how to inspect your feet every day for blisters, cuts, scrapes, and sores. Call your doctor promptly if you spot a red or inflamed sore.
Prevent trouble: You can protect your feet by wearing good-fitting shoes and clean socks at all times. Going barefoot -- even indoors -- is asking for trouble. Wash your feet every day, and carefully trim your toenails once a week. If you have a condition that would cause you to worry about injuring your toes clipping your toenails, ask your podiatrist to do the job. Most of all, try to keep your diabetes under control. If you can keep your blood sugar close to normal, your feet probably won't suffer from nerve damage or poor circulation, and a small injury isn't likely to become a big problem.








