If you’re wondering why you have to keep running to the bathroom even though you are limiting your intake of liquids and doing everything “right”, it could be your medicine. Yes, your medication can play a big role in how your bladder acts and what it needs to function properly–especially if that medication has nothing to do with your bladder. Here are some medications you may need to keep a close eye on to make sure they’re not contributing to your bathroom runs in the middle of the night.
If you’re wondering why you have to keep running to the bathroom even though you are limiting your intake of liquids and doing everything “right”, it could be your medicine. Yes, your medication can play a big role in how your bladder acts and what it needs to function properly–especially if that medication has nothing to do with your bladder. Here are some medications you may need to keep a close eye on to make sure they’re not contributing to your bathroom runs in the middle of the night.
9 Medications That Make You Go to the Bathroom
1. Diuretics
The point of a diuretic is to increase urination. “All diuretics work to increase the excretion of water and sodium from the body through the kidneys,” explains Dr. Hudspeth. This is helpful in treating conditions such as high blood pressure, swelling, heart failure, and liver or kidney disorders, she says. But peeing more can disturb your sleep if you’re waking up multiple times to go to the bathroom. Hudspeth recommends asking your doctor if you can take diuretics earlier in the day to avoid cutting into your sleep.
2. Tricyclic Antidepressants
Peeing is normally a well-orchestrated process. When your bladder fills up (and is holding that urine) the urethra — the tube connected to the bladder that empties urine — needs to stay shut to keep it all in until you decide you’re ready to go to the bathroom, says Hudspeth. What’s more, your bladder has to be able to contract to expel the urine into the urethra. Tricyclic antidepressants may interfere with both processes, and lead to leakage, also called urinary incontinence.
3. Antihistamines
For some people, sneezes can cause a little urine to leak. But this may also be due to an antihistamine that you’re taking to control allergy symptoms. The most common offenders are Benadryl (diphenhydramine) and Chlor-Trimeton (chlorpheniramine), says Jason Varin, PharmD, an assistant professor at the University of Minnesota College of Pharmacy in Minneapolis. “The bladder is a smooth muscle that fills up with urine. When it reaches a certain level and is full, it sends signals to the brain that it’s time to urinate,” he explains. Trouble is, certain antihistamines can relax the bladder, blunting its ability to push out urine. In the end, there is still some urine left in your bladder, which means it will fill up again faster and send that “gotta pee” signal to your brain sooner.
4. Decongestants
The good thing about decongestants such as Sudafed (pseudoephedrine) and Suphedrine PE (phenylephrine) is that they temporarily quell nasal congestion by constricting blood vessels, ultimately lessening swelling. But that effect happens to other muscles, too, including the bladder’s sphincter, says Dr. Varin. “This is the on-off valve of the bladder, and these medications may make the bladder constrict so that it’s more difficult for urine to pass from the bladder,” he says. In people with male genitalia, “decongestants can also constrict the prostate, which surrounds the urethra, also making it more difficult to pass urine,” Varin adds.
5. Calcium Channel Blockers
Among older adults who went to the doctor because of incontinence, 60 percent were taking medications that had urinary symptoms as a side effect, per a previous study. Among the most common medications they were taking? Calcium channel blockers. This class of medication, used to treat hypertension, may cause the bladder to relax and affect its ability to empty properly, says Hudspeth.
6. Mood Stabilizers
Lithobid (lithium) is a mood-stabilizing medication used to treat bipolar disorder, notes the National Alliance on Mental Illness (NAMI). “For some individuals, lithium is the best treatment, considered a lifesaver for some, even though it has a host of likely side effects,” says Varin. One of those potential side effects is excessive urination and thirst, which may affect up to 70 percent of individuals who take lithium long term, per a paper published December 2016 in the International Journal of Bipolar Disorders. While this side effect may be annoying, it can also be dangerous if the dose you’re taking is too high. “Lithium doses that are too high for an individual can lead to changes in the kidney and to a form of diabetes that impacts the function of the kidneys,” explains Varin. That condition is called diabetes insipidus, which is not the same as type 1 or 2 diabetes. “Diabetes insipidus has to do with the kidney’s ability to regulate fluids and reabsorb water properly, resulting in an increased urination of mostly fluids. In turn, that creates what some describe as an endless thirst,” he says. It can cause electrolyte and fluid imbalances, so talk to your doctor if you have these side effects.
7. Antipsychotics
Versacloz, FazaClo, and Clozaril (clozapine) are antipsychotic medications that treat schizophrenia, and can be a particularly important medication for patients who have suicidal thoughts, according to the U.S. National Library of Medicine. Frequent urination is one possible side effect because it can cause diabetes insipidus, says Hudspeth. One of the main complications of diabetes insipidus is dehydration, which has symptoms including thirst, dry skin, fatigue, dizziness, confusion, and nausea, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Talk to your doctor if you’re on this medication and experience increased urination.
8. Some Medications for Type 2 Diabetes
The newer medications for type 2 diabetes, a class called sodium-glucose cotransporter-2 (SGLT2) inhibitors work by “increasing the amount of glucose or blood sugar your kidneys excrete and pass through urine, which takes fluid with it,” says Varin. Some good news: There was a concern that SGLT2 inhibitors would also increase the risk of urinary tract infection (one symptom of UTI is a persistent urge to urinate, per the Mayo Clinic), but newer research has failed to find that connection, suggests the February 2020 issue of Clinical Kidney Journal.
9. Alpha Blockers
Alpha blockers, such as Cardura (doxazosin), Minipress (prazosin), and Hytrin (terazosin), are another class of medications used to treat high blood pressure. They work by relaxing blood vessels to allow for adequate blood flow — but they may also relax the muscles of the urethra and cause urinary incontinence, says Hudspeth. According to the Mayo Clinic, these drugs are often used in combination with other blood pressure lowering drugs, such as diuretics, so there’s a chance that increased urination issues could be caused by one or both these medications.
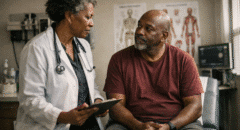
If you suspect medications may be worsening urinary leakage or even causing it, let your doctor know about all the medicines you take, both prescription and over-the-counter. That way, your doctor can help determine whether these medicines should be adjusted or stopped, or if a treatment should be modified.
If you have any concerns about your medication or new onset of urinary changes, speak to a primary care provider for an evaluation and medical guidance.