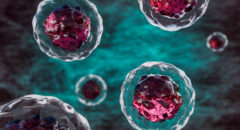
Stem cell transplants, also known as bone marrow transplants, have emerged as a revolutionary medical procedure with the potential to treat a variety of diseases, ranging from blood disorders to certain types of cancer. This cutting-edge therapy involves the infusion of healthy stem cells into a patient's body, aiming to replace or repair damaged cells and tissues. Let's delve into the intricacies of how stem cell transplants work and the transformative impact they can have on patients' lives.
1. Types of Stem Cell Transplants
There are two primary types of stem cell transplants: autologous and allogeneic. Autologous transplants involve the use of a patient's own stem cells, harvested and stored before undergoing treatment.
Allogeneic transplants, on the other hand, utilize stem cells from a donor, often a genetically matched family member or unrelated individual.
2. Preparation and Harvesting
Before a stem cell transplant, the patient typically undergoes a process called conditioning or pre-transplant therapy. This may involve chemotherapy, radiation, or a combination of both to eliminate diseased or malfunctioning cells.
In autologous transplants, the patient's stem cells are collected, or harvested, from their blood or bone marrow. For allogeneic transplants, the donor undergoes a similar harvesting process.
3. Infusion
Once the stem cells are harvested, they are processed and purified in a laboratory to ensure a clean and concentrated sample.
Subsequently, the patient or the recipient receives the stem cells through intravenous infusion. This marks the beginning of the transplant process, with the infused stem cells circulating in the bloodstream.
4. Hom-ing In
The infused stem cells navigate through the bloodstream to find their way to the bone marrow. This migration is a crucial step, as the bone marrow serves as the primary site for blood cell production.
Once settled in the bone marrow, the stem cells begin their work of generating new, healthy blood cells, including red blood cells, white blood cells, and platelets.
5. Engraftment
Engraftment is a critical milestone in the success of a stem cell transplant. It refers to the establishment of the donor's or patient's stem cells in the recipient's bone marrow and the production of healthy blood cells.
This process may take several weeks, during which time the patient is closely monitored for signs of engraftment and potential complications.
6. Recovery and Follow-Up
Following engraftment, the patient enters a recovery phase. During this time, the healthcare team monitors the patient's immune system, blood cell counts, and overall health.
The recovery period can vary depending on the type of transplant, the underlying condition being treated, and individual factors.
7. Potential Complications
While stem cell transplants offer hope for many patients, they are not without risks. Possible complications include graft-versus-host disease (GVHD) in allogeneic transplants, infections, and other side effects related to the conditioning therapy. Advances in medical research and transplant techniques aim to minimize these risks and improve overall outcomes.
Stem cell transplants represent a remarkable intersection of medical science and technology, offering a lifeline to individuals grappling with severe diseases. As our understanding of stem cells and transplantation techniques advances, the potential for these procedures to treat a broader range of conditions continues to grow. Stem cell transplants stand as a testament to the relentless pursuit of medical innovation, bringing new hope and healing to patients around the world.