 Tennis star Serena Williams battled it and it was the cause of the untimely death of rapper Heavy D and Tommy from the hit show “Martin”. And there are more people who are affected by this than we initially realized. The disease that is hiding is called Deep Vein Thrombosis (DVT).
Tennis star Serena Williams battled it and it was the cause of the untimely death of rapper Heavy D and Tommy from the hit show “Martin”. And there are more people who are affected by this than we initially realized. The disease that is hiding is called Deep Vein Thrombosis (DVT).
Currently, the Surgeon General’s Call to Action report highlighted the scope and impact seriousness of DVT. The report stated that as many as 180,000 to 300,000 deaths occur annually due to DVT and pulmonary embolism (PE) in the United States alone. Although many of these events are preventable, there are a large proportion of DVT events that occur spontaneously, without any signs or symptoms. This has led the Department of Health to make the prevention of this “silent killer” across the NHS a priority.
Some people do not know they have a DVT until the clot moves from their leg or arm and travels to their lung which can cause a pulmonary embolism.
How Common Is This Killer?
Each year, approximately 1 to 3 in every 1,000 adults develop a DVT or pulmonary embolism in the United States, and up to 300,000 people die each year as a result of DVT/PE. It’s the third most common vascular disease, behind heart attacks and strokes. Acute DVT/PE can occur at any age, but are less common in children and adolescents and more common in those over the age of 60. More than half of all DVTs happen as a result of being in the hospital from a medical illness or following surgery. The reason why DVTs are more common after a hospital stay is because you’re lying in bed most of the time instead of moving around like you normally would.
Symptoms You Should Worry About: Pulmonary Embolism
Symptoms of a pulmonary embolism include:
- Sudden shortness of breath or fast breathing
- Sharp chest pain that often comes with coughing or movement
- Pain in the back
- Cough (sometimes with bloody sputum/phlegm)
- Sweating more than normal
- Fast heartbeat
- Feeling dizzy or fainting
Symptoms You Should Worry About: DVT
Don’t let DVT get that far. Here are five of the top symptoms to look out for:
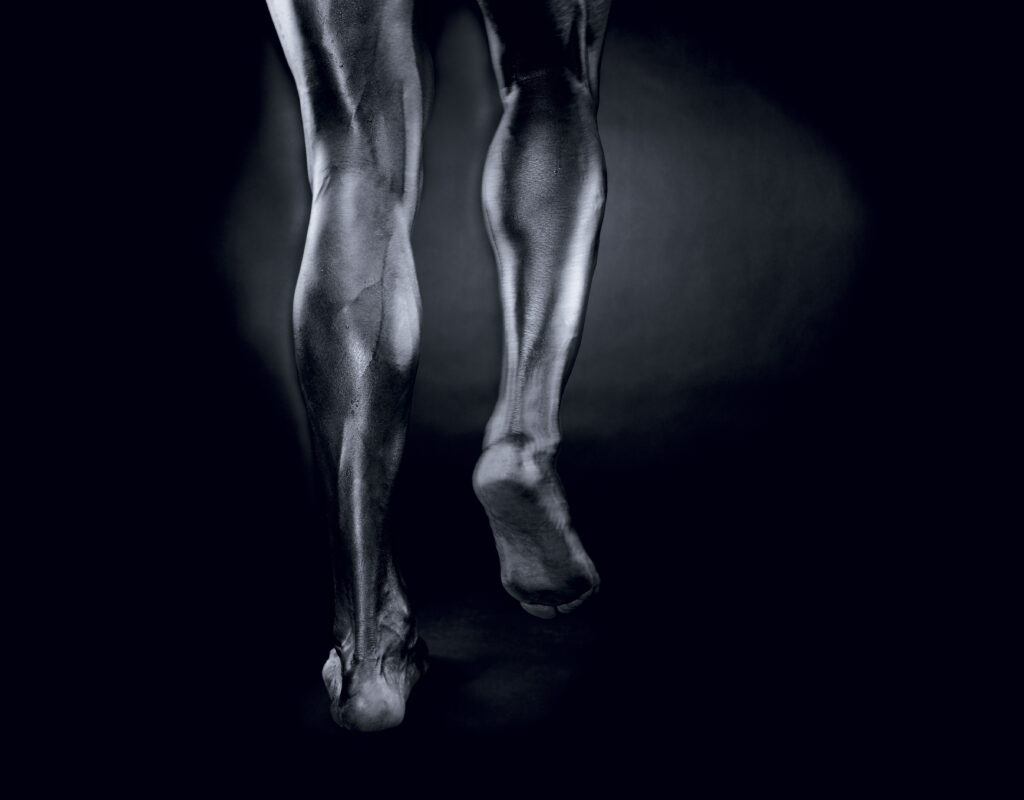
1. Leg Pain
With large blood clots, pain and tenderness can occur in the leg affected—particularly when standing, climbing stairs, or walking.
2. Swelling
Swelling, particularly around the affected area (i.e., calf or thigh) may occur with a worsening clot.
3. Feverish Skin
Another common sign shows itself in the affected leg with skin that is warm to the touch or even feverish.
4. Patchy Skin
The leg afflicted with the blood clot may also turn red and patches of discolored skin may develop along the thigh or calf muscle.
5. Bloody Coughing
Sudden and unexplained coughing may occur with bloody mucus within.

You Can Help Prevent It If you:
- Wear loose-fitting clothes, socks, or stockings.
- Raise your legs 6 inches above your heart from time to time.
- Wear special stockings (called compression stockings) if your doctor prescribes them.
- Do exercises your doctor gives you.
- Change your position often, especially during a long trip.
- Do not stand or sit for more than 1 hour at a time.
- Eat less salt.
- Try not to bump or hurt your legs and try not to cross them.
- Do not use pillows under your knees.
- Raise the bottom of your bed 4 to 6 inches with blocks or books.
- Take all medicines the doctor prescribes you.
What Is Your Estimated Risk?
Blood Clots: High Risk
-
- Hospital stay
- Major surgery, such as abdominal/pelvic surgery
- Knee or hip replacement
- Major trauma: automobile accident or fall
- Nursing home living
- Leg paralysis
Blood Slows: Moderate Risk
- Older than age 65
- Trips over 4 hours by plane, car, train, or bus
- Active cancer/chemotherapy
- Bone fracture or cast
- Birth control pills, patch, or ring
- Hormone replacement therapy
- Pregnancy or recently gave birth
- Prior blood clot or family history of clot
- Heart failure
- Bed rest over 3 days
- Obesity
- Genetic/hereditary or acquired blood clotting disorder
Blood Flows: Average Risk
- Active
- Younger than age 40
- No history of blood clots in immediate family
- No conditions or illnesses that heighten clotting risk
Practical Steps to Lower Your Risk
- Ask your doctor about need for “blood thinners” or compression stockings to prevent clots, whenever you are admitted to the hospital
- Lose weight, if you are overweight
- Stay active
- Exercise regularly; walking is fine
- Avoid long periods of staying still
- Get up and move around at least every hour whenever you travel on a plane, train, or bus, particularly if the trip is longer than 4 hours
- Point and flex your toes and make circles with your feet if you cannot move around while sitting for prolonged periods to get your blood circulating
- Stop at least every two hours when you drive, and get out and move around
- Drink a lot of water and wear loose fitted clothing when you travel
- Talk to your doctor about your risk of clotting whenever you take hormones, whether for birth control or replacement therapy, or during and right after any pregnancy
- Follow any self-care measures to keep heart failure, diabetes, or any other health issues as stable as possible
Visit the BlackDoctor.org High Blood Pressure center for more articles.