Earlier this summer, we reported on a flesh-eating bacteria that was threatening a few parts of the U.S. Now, the number of cases and reports of that deadly bacteria has grown.
More emergency alerts have gone out along the Southeast as Vibrio vulnificus, a dangerous flesh eating bacterium, has made an alarming comeback. Health officials in Louisiana, Florida, Mississippi, and Alabama are reporting a sharp rise in infections including multiple deaths far exceeding historical averages.
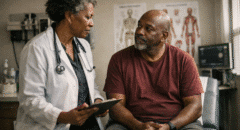
“This is a very scary-sounding bacteria, Vibrio vulnificus. Fortunately, it is rare, but it can be very deadly,” Dr. Alok Patel, ABC News medical contributor and pediatrician at Stanford Children’s Health, told ABC News.
“This bacteria normally exists in warm water, salty water, sometimes brackish water, especially during summer months,” Dr. Patel explained. Brackish water occurs where fresh water meets salt water.
What Is It and How Does It Get into Your Flesh?
Flesh-eating disease occurs when bacteria enter the body through a break in the skin. People with a weakened immune system can be at greater risk of developing this condition. Vibrio vulnificus is a species of Gram-negative, motile, curved rod-shaped, pathogenic bacteria of the genus Vibrio. It is present in marine environments such as estuaries, brackish ponds, or coastal areas.
The most common way to get it is when bacteria invade your body through a cut in your skin, although it can happen if you have a trauma that doesn’t break the skin.
Ways that bacteria can enter your skin:
- Cuts, scrapes or burns
- Insect bites
- Wounds from needles and other things that cause puncture wounds
- Surgery
- Food
- While Group A strep bacteria are the most common cause of necrotizing fasciitis, you can also get it from many different types of bacteria, including bacteria that live in water.
What Food Can You Find It In?
People can get infected with Vibrio vulnificus when they eat raw shellfish, particularly oysters. The bacterium is frequently isolated from oysters and other shellfish in warm coastal waters during the summer months. Since it is naturally found in warm marine waters, people with open wounds can be exposed to Vibrio vulnificus through direct contact with seawater. There is no evidence of person-to-person transmission of Vibrio vulnificus.
Symptoms You Need to Pay Attention To
Common gastrointestinal signs and symptoms of Vibrio infection:
- Watery diarrhea
- Stomach cramps
- Nausea
- Vomiting
- Fever
- Chills
Signs and symptoms of Vibrio wound infection:
- Fever
- Redness
- Pain
- Swelling
- Warmth
- Discoloration
- Discharge

Where are flesh-eating bacteria cases in the US?
Louisiana has reported the highest number of Vibrio vulnificus infections in a decade, with 17 reported cases and hospitalizations, including four deaths, as of July 30. This is compared to the 10 years prior, which saw an average of only seven cases and one death a year during the same time period.
Florida has likewise reported four deaths caused by Vibrio vulnificus infections as of July 24. The state has counted 13 total cases, a rate that isn’t necessarily abnormal at this point in the year, according to Florida health data.
An average of 150 to 200 cases are reported each year, with most of them in Gulf Coast states, according to CDC data.
If You Feel You May Have Been Infected through a Wound, Here’s What to Do:
Initiate treatment promptly. Do not wait for consultation with an infectious disease specialist or for laboratory confirmation of Vibrio vulnificus infection.
- Start antibiotic therapy.
- A third-generation cephalosporin (e.g., ceftazidime 1–2g IV/IM every 8 hours) plus doxycycline (100mg PO/IV twice a day for 7–14 days) is recommended.
- Alternate regimens include a third-generation cephalosporin with a fluoroquinolone (e.g., 500mg ciprofloxacin PO twice a day) or a fluoroquinolone given alone.
Children may also be treated with a third-generation cephalosporin plus doxycycline or a fluoroquinolone. However, doxycycline and fluoroquinolones are sometimes avoided in children due to concerns about side effects. Children may be treated with an alternative regimen of trimethoprim-sulfamethoxazole plus an aminoglycoside. Doses should be appropriately adjusted for renal and hepatic function.
- Consult your doctor and if appropriate, consult a microbiologist or infectious disease specialist.
- Give careful attention to the wound site.
- Necrotic tissue should be debrided.
How Can You Prevent It?
A few quick tips to fight it even before it can get to you:
- Do not eat raw oysters or other raw shellfish.
- Cook shellfish (oysters, clams, mussels) thoroughly.
- For shellfish in the shell, either a) boil until the shells open and continue boiling for 5 more minutes, or b) steam until the shells open and then continue cooking for 9 more
- minutes. Do not eat those shellfish that do not open during cooking. Boil shucked oysters at least 3 minutes, or fry them in oil at least 10 minutes at 375°F.
- Avoid cross-contamination of cooked seafood and other foods with raw seafood and juices from raw seafood.
- Eat shellfish promptly after cooking and refrigerate leftovers.
- Avoid exposure of open wounds or broken skin to warm salt or brackish water, or to raw shellfish harvested from such waters.
- Wear protective clothing (e.g., gloves) when handling raw shellfish.